Introduction
Polycythemia, characterized by elevated red blood cell count and hematocrit levels, affects approximately 3.4% of the population based on WHO 2016 criteria. However, existing studies predominantly focus on Caucasian populations, leaving a knowledge gap in Indian population data. Moreover, the emphasis on JAK2 mutation as a diagnostic marker has overlooked other potential risk factors like hypoxia induced sleep disturbances as causes for secondary Polycythemia. This study aims to fill these gaps by exploring the impact of overlooked risk factors and their association with polycythemia incidence.
Methods
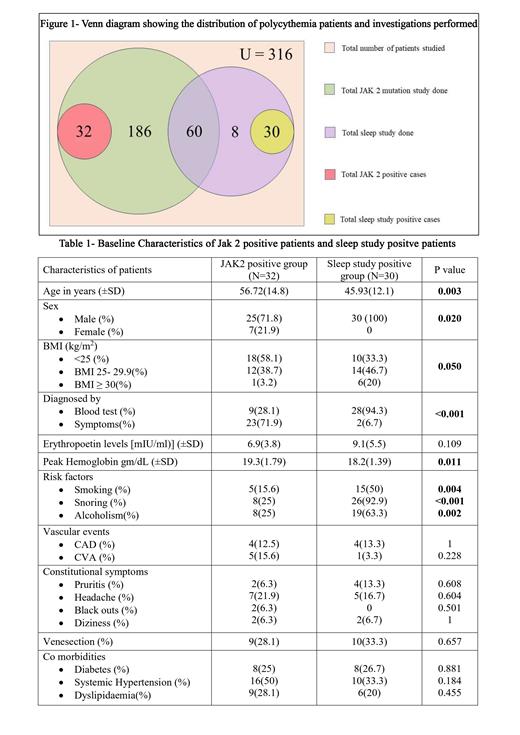
Clinical data from patients evaluated for Polycythemia at two tertiary care centers in south India between January 2021 and May 2023 were collected with Institutional Research Board approval (n=316). From all the Polycythemia patients who attended Hematology out patient department, two cohorts were identified: patients who underwent JAK2 mutation study and those who underwent a sleep study. Baseline characteristics, risk factors (e.g., smoking, snoring), comorbidities (diabetes, hypertension, dyslipidemia), constitutional symptoms (pruritus, headache, blackouts, or dizziness), and vascular complications (coronary artery disease or cerebrovascular events) were recorded. Additional details such as apnoea-hypopnea index (AHI) and nocturnal desaturation were documented for those patients who had undergone sleep study. Patients who were having moderate and severe AHI were considered as sleep study positive. As many were home sleep test and due to other patient related factors, using oxygen desaturation index for hypoxemia was not relied upon. Statistical analysis was conducted using Chi-square test and t-test for equality of means.
Results
A retrospective analysis of 316 patients with a diagnosis of erythrocytosis as per the WHO 2016 criteria (Figure-1) was done. Among them, 278 underwent JAK2 mutation study, with 32 testing positive. Meanwhile, out of the 98 patients who underwent sleep study, 30 tested positive. The probability of testing positive in a sleep study was higher than testing JAK2 mutation positive. Patients in the sleep study-positive group were significantly younger (mean age 45.93±12.1 years) compared to the JAK2-positive group (mean age 56.72±14.8 years) (p=0.003). The sleep study-positive group comprised of only males, while the JAK2-positive group included both males (71.8%) and females (21.9%) (p<0.05). In the sleep study group, most patients were diagnosed incidentally during routine blood investigations, while the majority in the JAK2-positive group presented with symptoms (p<0.001).There was a higher percentage of overweight (46.7%) or obese (20%) patients in the sleep study group, while the majority in the JAK2-positive group had a normal BMI (58.1%) (p=0.05). Co-morbidities were similar in the two groups leading to no significant statistical difference. Both groups required venesection without significant differences (Table -1).
Conclusion
Sleep study shows promise as a relevant diagnostic tool for certain cases of erythrocytosis. Patients who test positive for sleep study may differ from those with a positive JAK2 mutation in terms of age, gender distribution, BMI, and presentation. However, both groups share similar co-morbidities and initiation of venesection rates. The low incidence of JAK2 mutation in polycythemia patients necessitates the consideration of sleep study as an additional evaluation tool. Our study was limited by its retrospective nature. Moreover, many patients who had performed sleep studies had not done a JAK2 mutation test. Further research is needed to validate these findings and enhance the understanding of causative role of sleep apnoea in JAK2 unmutated polycythemia in Indian population.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal